Clinical Simulations In Nursing: Debriefing and Development Of Students’ Clinical Judgement Abilities
The project of clinical immersion simulation at Cégep de Sainte-Foy came into being following the withdrawal of the ECOS (Examen clinique objectif structuré) that the Ordre des infirmières et infirmiers du Québec used for the licensing exam. This exam served to assess the clinical judgement of graduating students in practical situations. Our department also used scenarios of the ECOS from previous years to assess the students at the end of each session while at the same time allowing them to prepare for the licensing exam at the end of their college courses.
Since the withdrawal of the ECOS in 2014, the licensing exam concentrates on the theoretical aspects of the nursing practice. As teachers, we found ourselves facing a void in terms of assessment of practical skills which was now limited to the internships in a hospital environment. However, exposure to the differing issues of the hospitalized clientele is not the same for all trainees. In that context, how would learning and assessment be standardized? That situation led us to adopt a different pedagogical strategy for the Nursing course of study: the high-fidelity clinical simulation.
A Necessary Space for The Practical Training of Future Nurses
In Nursing there is a critical need for practical training. Despite the theory and laboratories, the students do not always make the right connections between the notions learned. In a clinical environment, safety is our primary concern. Real lives are at stake: teachers and charge nurses cannot stop to explain to students why a patient’ s condition is deteriorating. Thus the students cannot always analyse their thought process and call into question the connections, sometimes faulty, that they make with the subject matter. For example, sometimes students develop automatisms and believe “ if I act this way with Ms. X, I can do the same for Ms. Y”. The context of their internship does not always offer students the opportunity to fully develop their critical judgement.
High-fidelity simulation provides space for a necessary reflection and the opportunity to develop good reflexes. Our objective with this approach is to help students practice more, reflect on their practice and transfer their learning to their internship.
Advantages and Pedagogical Objectives of The Clinical Simulation
Studies show that learning by simulation fosters a more efficient nursing care. Simulations significantly increase a nurse’s ability to recognize the signs of deterioration in a patient’s health, thus contributing to improve their chance of survival (Ozekcin, 2015). Furthermore, using simulations as an additional pedagogical activity can replace internship hours, without even affecting the success rate of the clinical skills assessment (Hayden, Smiley, Alexander, Kardong-Edgren and Jeffries, 2014).
The following table summarizes the pedagogical advantages of clinical simulation over internships in nurses’ training:
| The limitations of traditional clinical teaching (internship) | Pedagogical advantages of simulations |
|---|---|
| Exposure to patients in a clinical setting is random. | Simulations allow for standardized situations and learning. |
| The teacher’s time is mostly spent on the patients’ needs. | The debriefing that immediately follows a simulation becomes an excellent opportunity for an in-depth discussion with the students. |
| Achievement of certain competencies is more difficult to assess. | Simulations make it possible to assess:
|
| The safety of the patient or the student supersedes the development of competencies. | Students are exposed to different situations that provide the opportunity to explore various avenues in a safe context and in an autonomous manner. |
Visiting the Installations and Presenting Our Patients
The first challenge that presented itself was to find an appropriate physical location as well the necessary material to carry out the first clinical simulation tests. At first, we used a storage room in the college and we tinkered with a manikin, a computer and unused electronic devices. This low-fidelity manikin, that we named Mr. Francoeur, allowed us to carry out various nursing interventions:
- Taking blood samples
- Setting up an IV
- Any other care that does not require any technologies to detect medicine
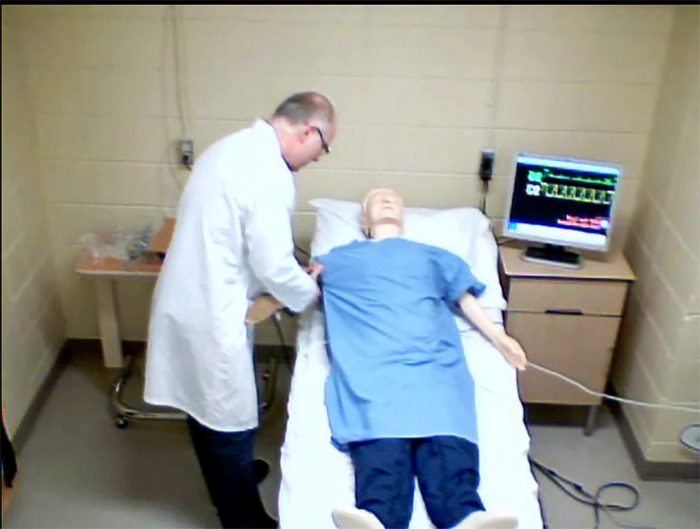
Yvon Brunet and Mr. Francoeur, the first manikin used for simulations at the Cégep de Sainte-Foy.
Since then, 4 high-fidelity manikins have been added to Mr. Francoeur:
- Hall is the most specialized, particularly in terms of the electronics used to detect pulmonary gaseous exchange.
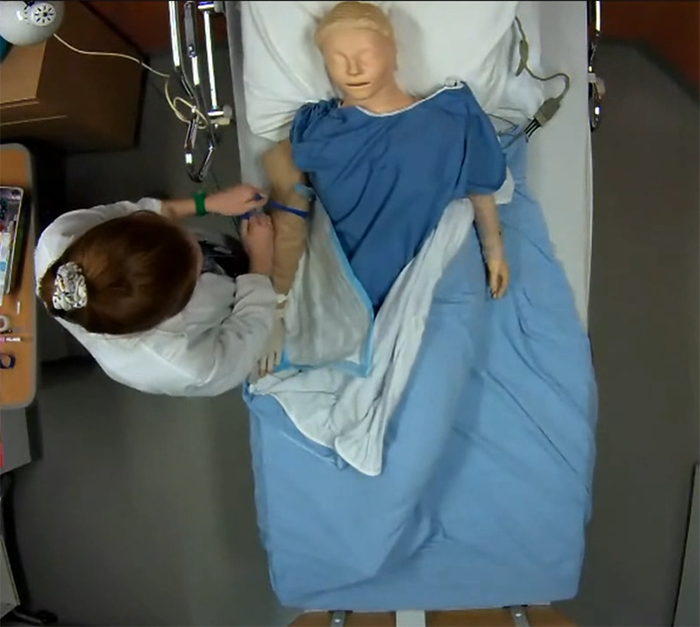
- Suzi is used mainly for nursing and allows students to do all of the tasks they could be required to do during their internship.
- Ped-Hall is a paediatric manikin that enables paediatric simulations without any risk to a young patient’s life.
- A neonatal manikin is used for newborn healthcare simulations and for neonatal intensive care simulations.
We also use actors for some simulations. For obstetrics, we bought a pregnancy prosthetic that an actress can wear to play a pregnant woman.
Before benefitting from our current installations, simulations were filmed with a camera on a tripod. Then the camera was plugged into a projector to see the relevant sequences. We now have 2 fully equipped simulation rooms with the computer hardware for recording. The 3 characteristics of the room layout:
- A simulation room where all of the necessary material (manikin, stretcher, etc.) is located.

One of the clinical simulation rooms at the Cégep de Sainte-Foy.
- A control room where the control room operator and the teacher interact during the simulation and make the video recordings.

A control room. The teacher and the operator can follow the simulation through a one-way glass and interact with the student through a microphone.
- A debriefing room where students observe their colleagues during the simulation. It is also in this room that the debriefing takes place using the video sequences.
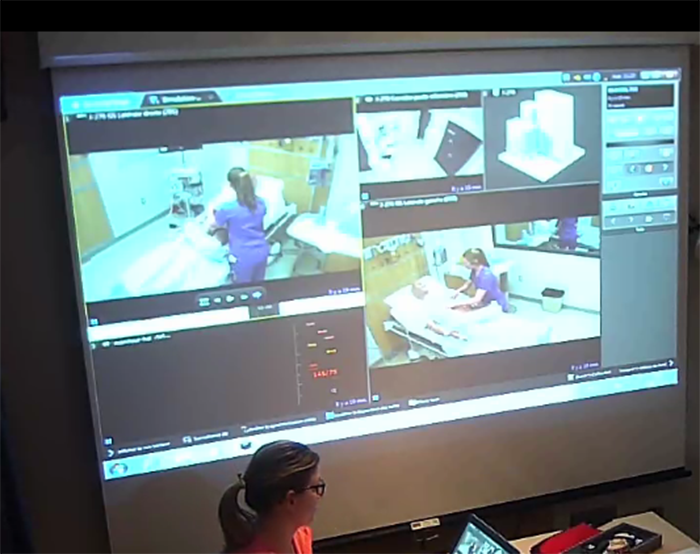
Students can watch their colleagues during the simulation on the screen in the debriefing room. Shots taken from various angles of the simulation room are available. During the debriefing, the recorded video sequences are projected on the same screen.
The debriefing room is also fitted out with cameras. Recordings of the debriefing sessions are used for teacher training and allow us to receive feedback on our academic interventions and allow us to improve.
The camera of the main doorway.
Throughout the steps leading to the purchasing of the high-fidelity equipment, the team of teachers at the Cégep ensured that pedagogical considerations remained central.
A room fitted out with high-tech equipment is nothing more than a room with high-performance tools. How will all of this material be used to develop the students’ skills?
How Simulations Are Conducted
The approach that was retained by our department is an evolving script with the same patient. The students should not intervene in the same manner in each scenario, but rather use what they saw during the previous scenario and apply specific interventions to their own simulation. For a group of 6 students, that allows us to see 6 case-based problems in the same day. In our pedagogical design, each simulation is divided into 3 phases.
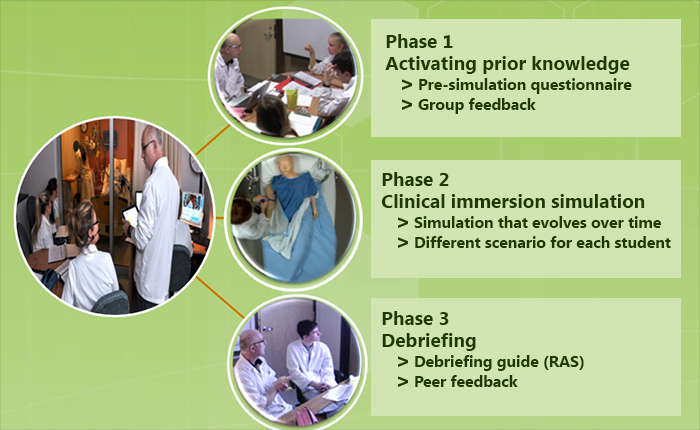
The 3 phases of the pedagogical design of clinical simulations in Nursing at the Cégep de Sainte-Foy.
Phase 1 – Activating prior knowledge
Using a questionnaire that the students previously filled in, we review the different theoretical and practical aspects related to a situation similar to the one the students will encounter during the simulation. I go around the table to validate the students’ answers and provide further information if necessary.
Phase 2 – Clinical immersion simulation
The students take turns conducting nursing interventions in the simulation room. Before starting, the students have 5 minutes at the “nurses’ station” to become familiar with the patient’s file, as they would at the beginning of a normal work shift.
The simulation lasts around 20 minutes, but even the time can be simulated (a scenario can take place during the night, for example). In the control room, I interact with the student by making the manikin speak or by playing the role of a doctor on the telephone, depending on the protocol.
The simulations are filmed from different angles. In the control room, I ask the person assisting me to place markers at key moments of the simulation recording to be able to come back to these precise sequences during the debriefing. The videos allow us to bring to light the passages that require the skill that we wish to develop in the students and that was targeted in the scenario.

Cardiac monitoring camera and lateral camera
Autopsy camera

Control room
During that time, the other students watch the simulation on a big screen in the adjacent room. They must be attentive to their colleague’s treatment techniques and jot down the good moves and not so good moves on the assessment grid that I provided.
Phase 3 –Debriefing and peer feedback
The student meets up with the group for the debriefing inspired by the PEARL Method. The debriefing is separated in 3 steps:
Self-assessment
The student is invited to express her feelings and to evaluate her performance. This can be an emotionally charged moment, especially if the simulation did not go well. Some students cry; others are disappointed with their performance and express this using humour or frustration. It is an essential step to free themselves of difficult emotions before the start of the debriefing and before receiving feedback from their peers.
Facilitation
This step consists in establishing the student’s intervention framework in order to identify what theoretical, practical or experiential knowledge the student mobilizes in response to the problems encountered during the simulation. To do so, I ask open questions related to the skills singled out in the scenario. The student must justify the nursing interventions that were used in relation to her understanding of the subject matter. I also use segments of the video recording so that the student can see the actions taken and explain the underlying reasoning. Some questions are more challenging, but the student must find, by herself, a way to modify her practices in the future. The objective here is not to give feedback but to guide the student’s reflection in a formative manner.
Feedback
The last step in the debriefing consists in a peer assessment of the technical elements, such as:
- Nursing care
- Nursing protocols
- Use of the material
- Questions patient was asked
These comments should be constructive. The students who were observing must put forward the things their colleague did well. It is all the more essential as the students coming out of a simulation tend to be a lot harder on themselves than the teacher or the other students would be.
From the pedagogical point of view, the debriefing is the most important part. It fosters retrospection and it is at this time that the student realizes her strengths as well as needs for further development. In assigning to the students the responsibility of assessing their colleague’s caregiving techniques, I can focus on the pedagogical framework while observing the student’s skills in the simulation room.
Support Learning By Allowing Students To Make Errors
The high fidelity manikin offers students the opportunity to see their errors. If a student wrongly identifies the symptoms or administers the incorrect dosage, the manikin’s condition will deteriorate. The debriefing then becomes a learning opportunity. My role is not to tell the student what she did wrong, but to question her on the reference framework that she uses in order to understand why she took those actions. Open questions make it possible to consider that aspect further. They give the student the opportunity to redefine her conceptual framework and improve her clinical judgement to transpose it eventually to the context of the internship.
When watching certain video sequences, the student is able to see the consequences of her errors. I present the important sequences independently of their success or failure.
It sometimes happens that students question a perfectly executed intervention while they are watching an extract of their simulation. In any case, I let the student express herself and analyse her intervention before I validate her actions or turn back to what should be improved.
If I notice a serious error, I remind the students of the good practices during the plenary. Sometimes, I give a “pedagogical prescription” for a student to review certain theoretical elements in more detail.
Following Developments In Clinical Simulation
A PAREA research is underway at Cégep Sainte-Foy in collaboration with the Cégep de Sherbrooke. The aim is to evaluate the effect of a sequence of teaching activities evolving over time during a clinical simulation in cardiology. The results of this research will be published in 2017.
Furthermore an interdisciplinary simulation committee was created in our college. It brings together the 3 health care programs:
- The department of inhalotherapy
- The department of pre-hospital emergency care
- The department of nursing
The teachers of these 3 programs received training on how to build a clinical simulation scenario and on good debriefing practices. The committee is the pillar and will help teachers develop and improve their scenarios during the steering process. From now until September 2018, our wish is to implement simulation as a pedagogical activity in our curriculum for all of the students in the nursing program.

